This is a full transcript of the testimony by our Executive Director, Peg Sandeen, at the February 28, 2020 hearing of the Maryland Senate Judicial Proceedings Committee in support of Senate Bill 0701, the End-of-Life Option Act. We have formatted the testimony and added subheadings for clarity.
*
My name is Peg Sandeen. I am testifying in support of Senate Bill 701, the End-of-Life Option Act. I am the executive director of the Death with Dignity National Center and a social worker with a PhD in Social Research.
I have more than 20 years of experience working directly with people who are terminally ill, including individuals who have opted to hasten their death using medication prescribed under death with dignity legislation.
In addition, I am an academic, an adjunct instructor of Social Work at Columbia University School of Social Work. I am not speaking on behalf of Columbia, but I note my role as an academic because I will be talking about several academic studies that demonstrate the soundness of death with dignity as a viable and well-researched public policy which is safe and effective.
Majority Support
I represent Death with Dignity and over 4,000 Marylanders, a number of whom are here today, who support the right of all individuals with a terminal illness to die on their own terms. Some of those supporters are dying themselves. People like Christine Hodgdon, a 39-year-old woman with metastatic breast cancer and a steadfast advocate for death with dignity. Like so many Marylanders who are moved personally by this issue, she submitted written testimony, and I hope you will take a moment to read her story.
Christine is but one of the strong majority of Marylanders who support this law. Recently, we commissioned a poll from Gonzales Research [1], a local polling firm, and the results show two-thirds of Marylanders support the End-of-Life Option Act.
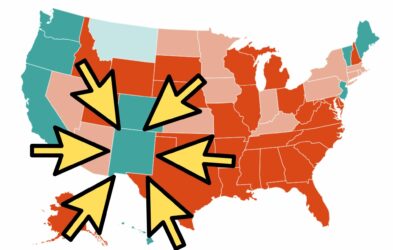
In fact, solid majorities of Maryland residents in all regions of the state, across the political spectrum, and from all demographic groups support this legislation. Gonzales Research queried likely voters and 60 percent of respondents in Western Maryland supported the law. Similarly, 65 percent of respondents in the Baltimore suburbs supported the law as did 67 percent of those from the Eastern Shore. In the Washington Metro area, a full 71 percent of respondents stated their support for medical aid in dying.
Two-thirds of Marylanders support the End-of-Life Option Act.
In my career working with people who are terminally ill and dying, I have come to believe that one of the most difficult things for a terminally ill individual is the silence arising out of society’s unwillingness to face death directly. Public conversations, of which testimony to a legislative body is a perfect example, provide an avenue for private conversations about dying to occur among family members.
At least one family in the state of Maryland tonight will have a difficult conversation about dying and last wishes and advance directives because they heard about this hearing today.
A Medical Standard of Care
The proposed law you are considering today is, at its core, a medical standard of care designed to provide physicians and pharmacists with best practice guidelines for situations in which a terminally ill and competent patient requests the right to control the timing and manner of his/her death.
Senate Bill 701 is modeled on legislation that has been enacted in nine jurisdictions, including your Washington, D.C. and New Jersey neighbors.
Beyond providing physicians with best practice guidelines, the End-of-Life Option Act puts decisions about easing suffering in the hands of terminally ill patients, allowing them to engage their family members, their physicians, clergy members and anyone else they choose, if they so choose.
It sets aside outdated and archaic government bans on a medical practice that is currently legal for 70 million Americans, a practice that is validated, researched, effective, and full of safeguards to protect vulnerable populations.
Numerous Safeguards
The multiple safeguards in Senate Bill 701 include:
- A diagnosis of a terminal illness with a prognosis of six months or less to live, verified by a second opinion.
- A mandatory counseling referral if either the attending or consulting physician believes the patient may not have capacity to make this health care decision.
- Oral and written request. The written request must be witnessed by at least two people, one of whom must be someone who is not a relative or an heir set to receive an inheritance from the individual. The physicians involved cannot be witnesses.
- Information must be provided to the patient on all forms of palliative care, hospice care, and other end-of-life options.
- The patient may opt out at any time and for any reason.
- The patient must self-administer the medication.
- Any health care professional or healthcare institution may choose not to participate.
To emphasize: No physician, pharmacist, nurse, or any type of care facility may be forced to participate. Whether by conscience, religious belief or moral objection, every person potentially involved in this process may refuse to participate.
The policy you are considering has been subject to independent research protocols by individuals from a myriad of academic disciplines. These researchers have examined the safeguards and demonstrated there have not been any instances of abuse or coercion of patients in the more than two decades since the law took effect. These findings over and over refute the arguments by opponents of death with dignity.
The Oregon Experience
Oregon has successfully implemented a death with dignity law for over 20 years. What do we know about the Oregon experience offering death with dignity with these same safeguards you are considering?
The law is rarely used. Statistics collected by the Oregon Health Authority [2] demonstrate only 1,459 individuals have ended their lives using the death with dignity law in 21 years. Every year, about one third of the individuals who go through the process to become qualified patients do not ingest the medication, but rather, go on to die from their underlying condition. Death with dignity for them is all about peace of mind.
The median age of participants is 74; 90 percent are enrolled in hospice; over 87 percent of them die at home; over 99 percent of them have insurance, either private or government sponsored. Overwhelmingly, these patients have cancer.
Oregon’s law has worked exactly as intended: to give dying and suffering patients more options at the end of life.
Opponents’ Claims Are False
Opponents of this legislation allege a lot of things this bill does and does not do. For more than two decades now, we have heard these same slippery slope arguments: statements that this law will target individuals who are poor or who are living with disabilities or the elderly; statements suggesting that those without medical care or access to healthcare resources will be forced to end their lives using medical aid in dying because it is cheaper than treating cancer.
These slippery slope arguments are just not true. Independent researchers have concluded that the results are quite the opposite.
In 2007, Battin et al. [4] explored data out of Oregon to determine if there was a disproportionate impact of 10 groups of potentially vulnerable patients. The data led the researchers to conclude
“…people who died with a physician’s assistance were more likely to be members of groups enjoying comparative social, economic, educational, professional and other privileges…there is no current factual support for so- called slippery-slope concerns about the risks of legalisation of assisted dying—concerns that death in this way would be practised more frequently on persons in vulnerable groups.” To reiterate, there is no current factual support for the slippery slope argument that vulnerable individuals are at risk for being coerced into using the law.
Law Complements Hospice, Palliative Care
Death with dignity also complements hospice and palliative care services. In a comprehensive study conducted with family members of 86 Oregonians who were participating in death with dignity, researchers concluded [5]:
“…another concern regarding the legalization of PAD [physician aid in dying] is that PAD would become a substitute for quality end of life care…Insofar as family rating of the quality of a loved one’s death is an indicator of end of life care, this study adds to the evidence that the choice to pursue PAD does not appear to be due to, or a reflection of, poorer end of life care.”
No Evidence of Coercion
Opponents of death with dignity spill 100 pills on a table, claiming that individuals using death with dignity must ingest all of them and asserting that the practice in Oregon was undignified. While visually startling, it is an outright untruth. No patient in any jurisdiction has been forced to ingest 100 pill capsules. It does not and cannot work that way.
Some claim a health insurance company denied them treatment, but offered medication to hasten death. It is true that insurance companies both deny treatment and cover the provisions under death with dignity laws, but linking them together to suggest that an insurance company would deny care and instead offer death with dignity, is a falsehood.
Not one of these claims has ever come to pass or been independently verified. Not in Oregon. Not in Washington State. Not in Vermont. California, Colorado, Washington, D.C., Hawaii, New Jersey, Maine. Nowhere.
Opt-Out Provisions
What we do know is that opposition to medical aid in dying comes largely from religious groups that say only God can decide when to end one’s life. That is why this law contains clear opt-out provisions for medical professionals and states that only those who meet the strict criteria and safeguards in this law will be able to receive this prescription.
Oregon Leads the Way
It is no coincidence that the very first state to pass death with dignity—Oregon—was recently identified in an article published in the New England Journal of Medicine [6] as a state with significant and positive differences in how people die, as compared with other states in the country. We do better than the rest of the country in such benchmarks as the number of people who die at home (as opposed to the hospital), the number of people using hospice, and the number of people who received intensive care services at the end of life.
The passage of our law and subsequent end-of-life policy changes sent a signal nationwide, and in Oregon, that dying patients must be accorded more and better care. Death with dignity is part of that equation.
A Strong Message
National research published in the New England Journal of Medicine indicates that physicians in every state, including Maryland [3], help patients die using prescription medication. By enacting this law, the Maryland Senate will send a strong message that a compassionate response to suffering is available in the state through medical aid in dying, but physicians must follow the carefully regulated safeguards you are considering today. The state of Maryland will shine a bright light on the process to ensure the protection of vulnerable individuals.
As legislators in this great state, if you want to improve the quality of life for dying individuals in your jurisdiction, there is nothing better that you can do than to enact a death with dignity statute. That’s what the data tell us. It will be rarely used, but a great source of comfort. Its safeguards will protect vulnerable individuals from coercion.
On Their Own Terms
Physicians in your state are already providing medications to patients to end their lives, but without state oversight. Medical aid in dying will likely improve the quality of end of life care for the whole population, not just for people who contemplate it or use it.
Like many other individuals with a terminal illness who have shared their stories with you and me, Christine Hodgdon cannot control the trajectory of her disease. But she should have control over the time and manner of her death: the right to die on her own terms, with autonomy and peace of mind.
It is time for dying patients in Maryland to have access to this end-of-life option.
I urge you to vote yes on Senate Bill 701.
Peg Sandeen, PhD, MSW
Executive Director
Death with Dignity National Center
References
[1] Gonzales Maryland Poll. Gonzales Research & Media Studies, January 2020.
[2] Oregon Public Health Division. Death with Dignity Act Annual Report, Year 21.
[3] Meier, D. E., Emmons, C. A., Wallenstein, S., Quill, T. Morrison, R. S., & Cassel, C.
K. (1998). “A national survey of physician-assisted suicide and euthanasia in the United States.” New England Journal of Medicine, 338(17), pp. 1193-1201.
[4] Battin, M. P., van der Heide, A., Ganzini, L, van der Wal, G., & Onwuteaka-Philipsen,
B. D. (2007). “Legal physician-assisted dying in Oregon and the Netherlands: Evidenceconcerning the impact on patients in ‘vulnerable’ groups.” Journal of Medical Ethics, 33, pp. 591-597.
[5] Smith, K. A., Goy, E. R., Harvath, T. A., & Ganzine L. (2011). “Quality of death anddying in patients who request physician-assisted death.” Journal of Palliative Medicine, 14(4), pp. 1-6.
[6] Tolle, S. W., & Teno, J. M. (2017). “Lessons from Oregon in embracing complexity inend-of-life care.” New England Journal of Medicine, 376(11), pp. 1078-1082.
No comments.