Our partner organization, End of Life Choices New York (EOLCNY) is one of the oldest state-based Death with Dignity organizations in the country. For the past 18 years, EOLCNY staff and volunteers have worked with a diverse array of individuals and organizations to educate policymakers, medical professionals, and the general public about a wide range of end-of-life options and to provide counseling for terminally ill patients.
The nonprofit has also been at the forefront of advocating for assisted dying in the Empire State. We are working with EOLCNY and Death with Dignity-Albany to promote A 2383, the Medical Aid in Dying Act. We spoke with EOLCNY Executive Director Laurie Leonard and Executive Director Emeritus David C. Leven, JD, about their advocacy and education work in 2018.*
Death with Dignity National Center: What is the current political climate in New York with regard to Death with Dignity?
Laurie Leonard: There is widespread support for medical aid in dying in New York. Almost 80 percent of the population is in favor; even among Republicans and Catholics, support ranges from 72 to 75 percent. We have a need not so much to convince lawmakers that passing Death with Dignity legislation is the right thing to do, but to reassure them that this is what most of their constituents want.
David Leven: Aid-in-dying legislation has been pending for 3 years now. The bill was amended in response to concerns raised by supporters and some opponents. We were involved in drafting the bill and the amendments. When one looks at the legislation itself, there are so many safeguards to protect both patients and healthcare professionals.
The experience with medical aid in dying in those states which have enacted legislation, including Oregon, which has over 20 years of experience with the law, has been extremely positive. None of the problems anticipated by opponents have arisen. There are a number of safeguards in the Oregon law, virtually none of which are required for people to make decisions to hasten their death by other means.

End of Life Choices New York Executive Director Emeritus David C. Leven, JD (center, holding microphone) speaks at a Death with Dignity debate arranged by the Sheen Center in New York City, in 2015.
Death with Dignity National Center: As is true in any state where Death with Dignity legislation is proposed, opponents to A 2383 have come out in force. Who are your most formidable opponents?
David Leven: New York has a powerful state Catholic Conference. It has been opposed to medical aid in dying and has considerable influence when it comes to health policy.
The Medical Society of the State of New York remains opposed. Hopefully it will take a neutral position soon and follow in the footsteps of the Massachusetts and Vermont Medical Societies, which shifted to a neutral position last year.**
We are fortunate to have the Chair of the Assembly Health Committee, Assemblyman Richard N. Gottfried, as a major supporter who has been involved in amending the bill. We are trying to get the bill out of that committee this session; it would be an important first step for us. It helps to have a supportive legislator in an influential position, especially when the opposition to this bill is formidable.
Death with Dignity National Center: In addition to building positive relationships with legislators, what are some of the most effective ways you have been able to engender support for Death with Dignity?
Laurie Leonard: One of the most effective ways to bring about change is for people whose family members have had very bad deaths to share their personal stories with the public.
Recently we commissioned a play based on the story of a man’s girlfriend’s illness and death. People who saw the play last year were deeply moved. Some of them told us that watching the play made them more supportive of medical aid in dying then they were before.
There is so much more support now for medical aid in dying than there was 16 years ago across the public, in the medical profession, even many religious organizations to a certain extent are more in favor of the practice. There is considerably more openness to discussing end-of-life issues more generally.
Death with Dignity National Center: Your work involves more than helping to draft and advocate for the passage of assisted-dying legislation. Can you share more about your latest educational and advocacy initiatives?
Laurie Leonard: In addition to advocacy, we provide educational presentations on advance directives, hospice and palliative care, and treatment alternatives at the end of life. Last year we gave 51 presentations to the public, graduate students, and healthcare professionals.
Last year we were authorized by the state Department of Education to develop workshops for social workers. Doctors usually don’t have the time or inclination to talk with patients about end-of-life issues, so these workshops are a critical resource.
Our Clinical Director, Judith Schwarz, has provided the bulk of our end-of-life counseling services for nearly 15 years. We have myriad testimonials from people that say how much they get out of her work with them on end-of-life options. She has developed an advance directive for Alzheimer’s patients that is much more comprehensive and thorough than anything we’ve seen thus far.
Finally, we received a grant in December to do education on end-of-life topics to Spanish-speaking individuals in New York City. Our Director of Outreach and Education, Ayana Woods, is overseeing a needs assessment and meeting with Latino leaders to understand the unique needs of the Spanish-speaking population. She also hired a bilingual educator to help us with our outreach efforts.

End of Life Choices New York Executive Director Laurie Leonard and Outreach and Education Director Ayana Woods at the New York State Capitol building in Albany, in 2017.
Death with Dignity National Center: Are you working on any legislation besides the Medical Aid in Dying Act?
David Leven: We continue to work on legislation focused on end-of-life issues beyond medical aid in dying. One bill we’re working on would prohibit healthcare providers from getting reimbursed for unwanted medical treatment. We’re beginning to work on a bill that would require hospitals as well as doctors when they realize that a patient has a terminal illness to offer the patient information and counseling on palliative care options and hospice. Another bill aims to increase the number of people who have completed healthcare proxies by requiring doctors to offer patients healthcare proxy documents.
We have been very successful over the years in getting legislation passed, particularly in the area of palliative care. We are hopeful that our current efforts will likewise prove fruitful.
Death with Dignity National Center: David, you have been on the front lines of the Death with Dignity movement for well over a decade. What changes have you seen in that time, and what gives you hope for the future of the movement?
David Leven: There is so much more support now for medical aid in dying than there was 16 years ago across the public, in the medical profession, even many religious organizations to a certain extent are more in favor of the practice. There is considerably more openness to discussing end-of-life issues more generally.
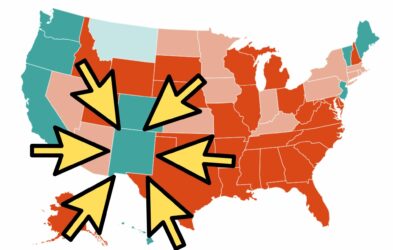
The fact that there’s been a number of states which have now enacted medical aid in dying in the past few years proves that this is an issue which is going to become much more recognized and accepted across the nation in the future.
Death with Dignity National Center: Laurie, what do you see as essential to growing support for Death with Dignity nationwide?
Laurie Leonard: There’s going to be a tipping point. When a certain number of states have legalized medical aid in dying, we will see a rapid succession of other states do the same. A large part of what’s driving greater interest in medical aid in dying is demographics: the Baby Boomers are getting older, and a large swath of the population is dealing firsthand with these issues. That has brought the issue to the forefront as never before.
* Interview edited for length.
** The New York Medical Society in 2017 resolved to conduct a survey among its members on the issue.
One comment.
JAMES LEONARD PARK
One proposed item of legislation for New York State
—Pre-Admission Notice of Policies on Respecting Patient’s Treatment Wishes—
might be expanded to include the requirement that all health-care institutions
that take care of dying patients MAKE PUBLIC their policies
with respect to which end-of-life medical treatments they will permit
and which life-ending decisions they will not allow under their care.
Read more about the specific medical methods of managing dying
that should be addressed in any such public statement
Comments are closed.