This is a full transcript of our Executive Director Peg Sandeen’s testimony at today’s (May 10, 2017) hearing of the Nevada State Senate Committee on Health and Human Services in support of SB 261, an assisted death bill. We have formatted the testimony and added subheadings for clarity.
*
My name is Peg Sandeen, and I am pleased to provide my testimony to the Committee today. I am a social worker with a PhD in Social Research, and I have more than 20 years experience working directly with people who are terminally ill. I am an Oregonian, and the Executive Director of the Death with Dignity National Center. I am here to share with you our experiences in Oregon, having successfully implemented a Death with Dignity law for 20 years.
The proposed law you are considering today is, at its core, a medical standard of care designed to provide physicians and pharmacists with best practice guidelines for the situations in which a terminally ill and competent patient requests the right to control the timing and manner of his/her death. National research published in peer-reviewed medical journals indicates that physicians in every state, including Nevada, help patients die through the use of prescription medication. By enacting this law, the Nevada Assembly will send a strong message that a compassionate response to suffering is available in the state; a law that contains significant and carefully regulated safeguards to protect patients and prevent misuse.
Death with Dignity puts decisions about easing suffering in the hands of terminally ill patients, allowing them to engage their family members, their physicians, clergy members, and anyone else they choose, if they so choose.
False Accusations About the Law
Today you are going to hear a lot of accusations about what this bill does and does not do. For two decades now, we have heard these same slippery slope arguments: statements that this law will target individuals living with disabilities or the elderly, and allegations about family members taking advantage of dying relatives. You may see someone spill 100 pills on the table, claiming that individuals using Death with Dignity must ingest all of them.
You may even hear testimony from someone claiming that a health insurance company denied treatment, but offered medication to hasten death. It is true that insurance companies both deny treatment and cover the provisions under Death with Dignity laws, but linking them together to suggest that an insurance company would deny care and instead offer Death with Dignity, is a falsehood. Not one of these claims has ever come to pass or been independently verified. Not in Oregon. Not in Washington State. Not in Vermont. Nowhere.
Oregon’s law has worked exactly as intended, to give dying and suffering patients more options at the end of life.
Opposition to this law comes largely from religious groups that say only God can decide when to end one’s life. That is why this law contains clear opt-out provisions for medical professionals and states that only those who meet the strict criteria and safeguards in this law will be able to receive this prescription.
Safeguards in SB 261
Throughout this law you will see a series of safeguards designed to protect the patient, the health care professional, and the family, all designed to ensure that the patient is in control. No one else but the patient may administer the medication.
The multiple safeguards in this proposed legislation include:
- A diagnosis the patient is within six months of death verified by a second opinion.
- A mandatory counseling referral if either the primary or attending physician believes the patient may not be competent to make this health care decision.
- Two oral and one written request. The written request must be witnessed by at least two people, one of whom cannot be the physician, a family member or someone who might receive an inheritance from the individual.
- Two waiting periods, 15 days between oral requests and at least 48 hours after the written request.
- An independent meeting with the physician to ensure the patient is not being forced or coerced.
- Information must be provided to the patient on all forms of palliative care, hospice care and other end-of-life options.
- The patient may opt out at any time and for any reason.
- The patient must self-administer the medication.
- Any health care professional may choose not to participate.
I want to reiterate that last point. No physician, pharmacist, nurse, or any type of care facility may be forced to participate. Whether by conscience, religious belief or any reason, every person potentially involved in this process may refuse to participate.
The Oregon Experience
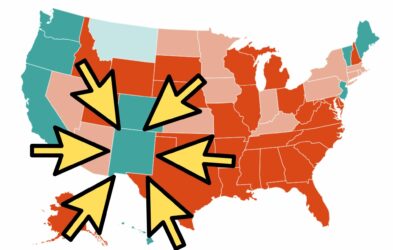
It is no coincidence that the very first state to pass Death with Dignity—Oregon—was recently named in an article by the New England Journal of Medicine as the state where more people die at home or in hospice than any other state. The passage of our law sent a signal nationwide, and in Oregon, that dying patients must be accorded more and better care that they control. We’ve responded in Oregon. And other states are now following our lead.
You will hear from a lot of people today who want to tell you about the Oregon experience. But in almost every legislative hearing I’ve attended, none of these people are from Oregon. I’ve worked with this law and the people who use it for 20 years. Oregon’s law has worked exactly as intended, to give dying and suffering patients more options at the end of life.
We very much appreciate Senator Parks for his strong support of this legislation and our organization stands ready to help Nevada become the next state to adopt a Death with Dignity law.
Thank you.
No comments.